To make a baby, sperm journey to an egg by swimming through the vagina, cervix, uterus, and then the fallopian tubes. Not exactly an epic quest to Mordor, but certain obstacles can make this journey difficult.
If you need some help on your expedition to parenthood, that’s where fertility treatments like intrauterine insemination (IUI) can help.
What is IUI exactly?
Intrauterine insemination (IUI) is a fertility treatment where a doctor inserts sperm directly into the uterus during ovulation. This gives sperm a faster route to the egg.
IUI is most often used by couples struggling to get pregnant or folks using a sperm donor.
Starting the journey: IUI uses
Just like therapy or clothes (looking at you, Brandy Melville), IUI isn’t one-size-fits-all. Here are a few reasons folks might opt for the fertility treatment.
- Unexplained infertility. Having probs getting pregnant, but can’t figure out why? You might be diagnosed with unexplained infertility. Folks with unexplained infertility and functionally normal fallopian tubes are particularly good candidates for IUI.
- Sperm donor. Whether you’re in a same-sex relationship or want to have a babe without a partner, IUI is great for those who want to use a sperm donor.
- Endometriosis-related infertility. Women who have minimal to mild endometriosis with normal pelvic anatomy are candidates for IUI. According to 2014 research, endometriosis could be to blame for 5 to 15 percent of infertility cases. Other research thinks it could even be up to 50 percent.
- Male-factor infertility. A male partner with moderate male-factor infertility is a good candidate for IUI. But if sperm count is too low or sperm abnormalities too severe, experts say that IUI has limited use.
- Cervical-factor infertility. This means sperm can’t swim through cervical mucus (basically discharge from the cervix) to meet the egg. Sometimes it’s because the mucus is abnormal — either too thick or thin. IUI helps increase pregnancy odds by bypassing this fluid.
- Ovulatory-factor infertility. About 25 percent of infertility cases are due to ovulatory factors, such as a reduced number of eggs or total absence of ovulation. IUI remains the first-choice treatment for ovulatory dysfunction.
- Semen allergy. An allergy to semen is rare. But when it happens, the allergic reaction may be avoided by implanting the sperm directly in the uterus.
Who isn’t a candidate for IUI?
Unfortunately, IUI won’t work for:
- females with moderate to severe endometriosis
- females who have had both fallopian tubes removed or blocked
- females with severe fallopian tube disease
- females with multiple pelvic infections
- males who produce no sperm (unless a sperm donor is used)
So how does the IUI procedure work?
While the procedure will vary based on your doc’s specific assessment and instructions, in general, here’s what to expect.
Prepare: IUI prep
Tracking ovulation
The IUI procedure must be synced around ovulation (when you “hatch” that egg 🥚).
You can pinpoint ovulation using at-home urine ovulation predictor kits. Or, you may visit the fertility clinic for bloodwork and ultrasounds to determine ovulation timing.
What route’s right for you will depend on your unique needs and your doc’s advice. Either way, you’ll work with your doc to schedule your IUI procedure around the time of ovulation.
Other fertility treatments
IUI can also be combined with fertility drugs designed to stimulate egg production and encourage ovulation.
Meds to boost your odds of getting pregs with IUI might include:
- Clomid
- Femara
- trigger shots containing human chorionic gonadotropin (hCG) or GnRH agonist
- follicle stimulating hormone (FSH) injections
If you’re taking meds, IUI is typically scheduled 10 to 16 days after starting them (and depending on your ovulation test results).
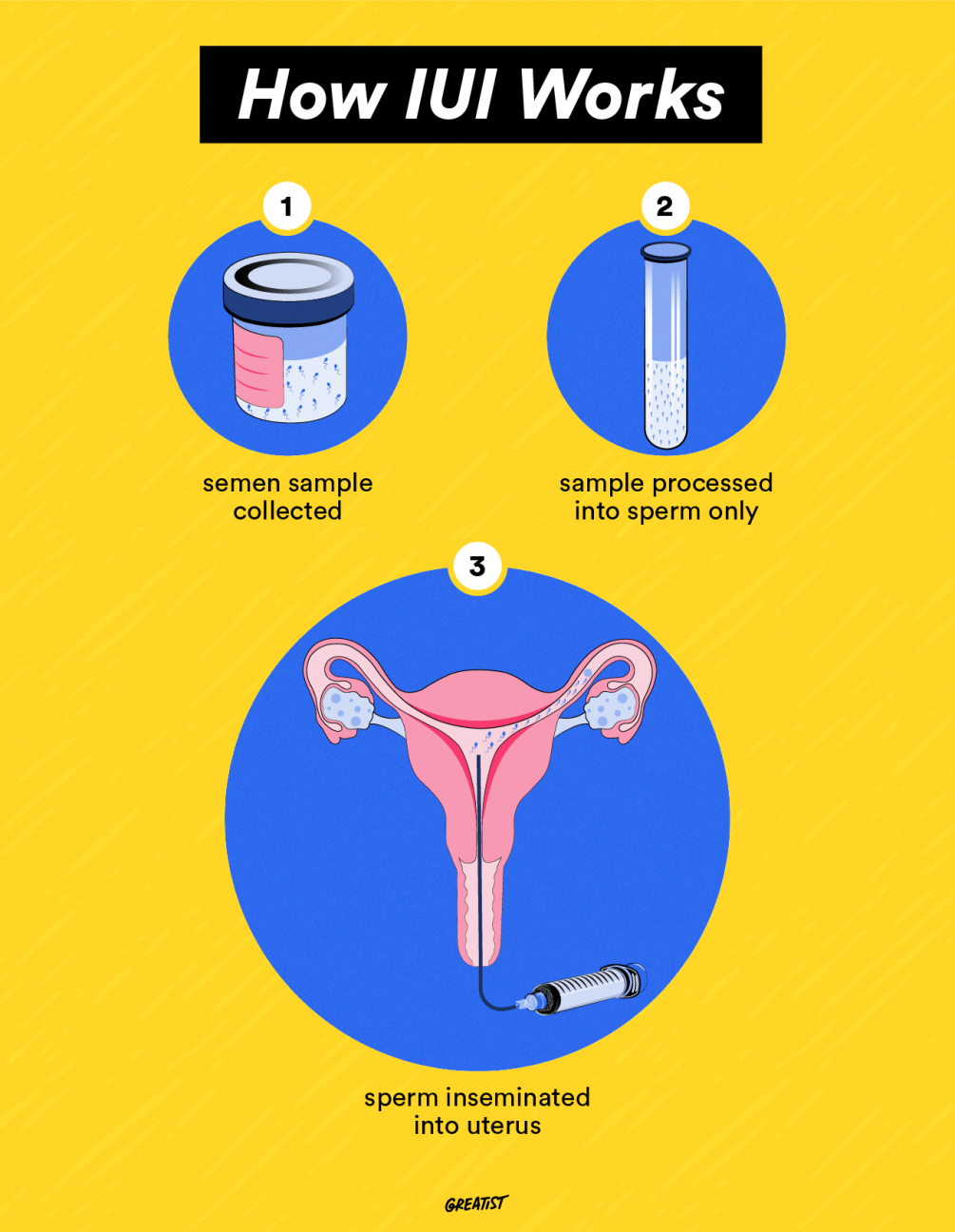
Semen sample
If a male partner is involved, he’ll provide a semen sample the day of the procedure. Otherwise, donor sperm will be thawed 🥶.
The semen sample is then taken to lab where each tiny swimmer will be “washed.” Basically, this means seminal fluid and other irrelevant debris are removed. As a result, the sperm is super potent and unlikely to bother the uterus with extra substances.
Showtime: IUI procedure
The actual IUI procedure takes about 15 to 30 minutes and doesn’t require any anesthesia or pain meds. Here’s what to expect on the big day:
- You’ll lie on the exam table with your legs in stirrups. Your doc will then use a speculum (you know, that metal pap smear tool) to open up the vagina.
- Your doc will insert a long, skinny tube attached to a syringe through the cervix and into the uterus. Once in place, they will inject the sperm.
- You may be asked to hang out reclined on the table for a few minutes.
- In some cases, the doctor will perform a second insemination the next day to boost your pregnancy odds.
Recovery: Post IUI care
Some people experience mild cramping or light bleeding after IUI. Otherwise, you shouldn’t experience any pain or discomfort after the procedure. You can go to work, hop on your elliptical, and live life as usual.
About 2 weeks after the procedure, cross your fingers and grab your pee sticks: it’s time to take a pregnancy test.
If there’s indeed a bun in the oven, some docs might prescribe progesterone to encourage a healthy pregnancy (depending on your unique fertility sitch).
Does IUI come with any risks?
IUI is considered a safe fertility treatment. Still, there are a few potential risks to keep in mind, especially if you’re pairing IUI with fertility drugs.
- Infection. Though there’s a small risk of infection post-IUI, it’s unlikely. Your doc uses sterilized instruments, so infection is rare.
- Multiple babies. Using fertility medications containing gonadotropins up your odds of conceiving multiples 👨👩👧👦 (not IUI itself). Multiple pregnancies carry heightened risks like premature birth, low birth weight, or death.
- Ovarian hyperstimulation syndrome (OHSS). Fertility meds can cause your ovaries overrespond to extra hCG, causing them to swell and fill up with fluid. OHSS is pretty rare, but it can be a medical emergency.
OHSS side effects
If you’re taking fertility meds for IUI and experience any of the following symptoms of OHSS, call your doc immediately:
- lightheadedness or dizziness
- sudden/rapid weight gain of more than 5 pounds
- shortness of breath
- nausea or vomiting
- severe ab or pelvic pain
- sudden increase in abdominal size
How much $ will IUI cost you?
Bank accounts, rejoice! IUI’s way less expensive than fertility procedures like in vitro fertilization (IVF). But, it’s still gonna cost you some green for fertility testing, prep, and the procedure itself 💵.
Depending on your insurance coverage and doctor’s fees, IUI generally costs about $300 to $1,000 without insurance (not including ultrasounds, lab tests, or semen analysis). For comparison, IVF can cost up to $15,000 or more out-of-pocket.
Some states have laws that make health insurance companies pay for some or all of fertility treatment if you meet certain requirements. Others offer zilch. If you’re not sure about your options, check out The National Infertility Association to learn more about coverage in the U.S. and chat with your insurance provider.
What’s the IUI success rate look like?
The success rate of IUI depends on a few factors, including:
- age (less effective for those over 40, especially after 3 cycles)
- the underlying infertility diagnosis
- whether fertility drugs are used
Overall IUI’s success rate per cycle isn’t super high compared to fertility treatments like IVF. But since IUI’s a lot cheaper and less invasive, doctors often recommend it before trying IVF. Let’s look at some stats 🔎.
According to a 2013 study, IUI success rates varied from 5 to 15 percent per cycle in women under 40 (up until the 6th cycle). A 2017 review estimated IUI’s success rate was about 10 to 20 percent per cycle.
For reference, a healthy 30-year-old woman has about a 20 percent chance of getting pregnant each month. IUI’s success rate isn’t really that different, but it might give folks facing infertility a boost to “normal” conception odds.
Do fertility drugs put the odds in your favor?
Pairing IUI with other fertility treatments may help your chances of pregnancy depending on your situation.
In a 2015 study, women with unexplained infertility who took Letrozole or Clomid with IUI had pregnancy success rates from 15 to 25 percent after 3 cycles. A 2017 study also found Letrozole was more successful than Clomid — and with fewer side effects.
Bottom line
IUI is a lower cost, low risk fertility treatment. It can be paired with or without fertility meds and is often an early treatment option for infertility. It’s also an option for folks using a sperm donor.
Having trouble getting preggo and wondering if IUI might work for you? Chat with your OB-GYN or a fertility specialist about your options.

0 Commentaires