Endometriosis is a pain — quite literally. If your periods are heavy and painful AF, it’s possible endometriosis is to blame for your period probs.
The American College of Obstetricians and Gynecologists estimates that 1 in 10 women of reproductive age have endometriosis, so you’re def not alone.
So what is endometriosis?
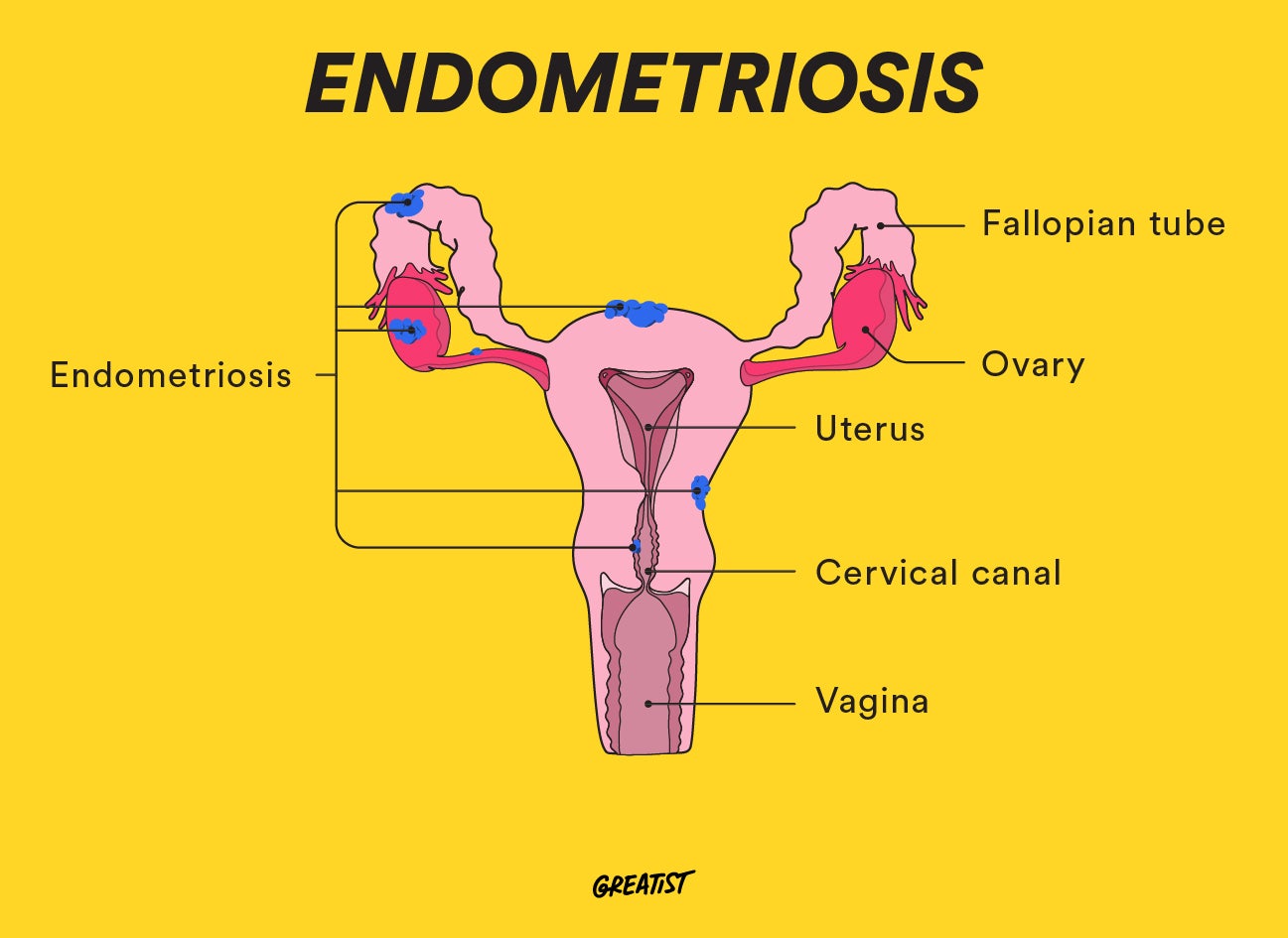
Endometriosis — “endo” for short — is a condition in which tissue similar to the lining of your uterus (endometrial tissue) grows outside its designated area.
You’ll generally find this rogue endometrial tissue on your ovaries, bowel area, or pelvic tissue. In rare cases, it can even grow in areas outside the pelvic region, like your urinary tract, gastrointestinal tract, and chest.
The condition is known mostly for causing pain and fertility issues, but it can also lead to scarring, irritation, and adhesions (tissue growths that bind your pelvic organs together).
Yikes! All this sounds super scary up front, but don’t fret. Treatment and support are available to help you manage endo symptoms.
Here’s the lowdown on everything endo.
Endo feels: What endometriosis symptoms can you experience?
While pelvic pain is the most common endo symptom, you may also experience:
- lower abdominal pain before or during your period
- heavy bleeding during periods
- bleeding between periods
- painful periods
- pain after sex
- pain when pooping
- lower back pain
- leg pain
Heads-up: The severity of these symptoms can vary!
Some folks may experience mild symptoms or none at all, while others have moderate to severe symptoms.
The intensity of your endometriosis symptoms has no bearing on the stage or degree of your condition. You could have a severe form of endo and barely notice your symptoms, or you could have a mild form and deal with awful pain or discomfort.
No matter the severity, you should see your gyno on the regular to monitor endo for any changes or complications.
Why TF is this happening?! Endometriosis causes
No one knows exactly what causes endometriosis 🤷♀️. But researchers have several theories as to why the condition *might* be wreaking havoc on your bod.
Retrograde menstruation
This is when menstrual blood doesn’t exit via your vagina but instead flows back through your fallopian tubes into your pelvic cavity. Research suggests that about 90 percent of people with periods will experience retrograde menstruation, but most don’t get endo.
Abdominal tissue transformation
Experts don’t fully understand why this happens, but sometimes small areas inside the abdomen turn into endometrial tissue. One theory is that this happens because abdominal cells are grown from embryonic cells, which can change shape and mimic endometrial cells.
Hormone probs
Hormones may be able to transform cells outside your uterus into endometrial cells. But there isn’t solid research to back up this theory.
Lymphatic system issues
Endometrial cells can be carried out of your uterus via your lymphatic system, which is how these cells end up way beyond your uterus.
Genetics
Several studies have suggested endometriosis might be hereditary since it pops up in families. If your mom, sister, or aunt has endo, it could be in your gene pool. (No thanks, Mom.)
The Mullerian theory
Maybe you’re born with it? This theory proposes that endo might start up while you’re in the womb. The idea is that cell tissue can get misplaced in response to puberty hormones while you’re just hanging out in utero.
Surgery complications
While this is super rare, it’s possible to get endometriosis after a cesarean delivery or a hysterectomy. These types of surgeries might allow endometrial cells to attach to scar tissue and spread to other parts of your body.
Immune system conditions
Hypothyroidism, fibromyalgia, and rheumatoid arthritis have been linked to endometriosis. This connection hasn’t been totally explained, but researchers think the inflammation caused by endo might trigger an immune system response.
Is it endo or something else?
Endometriosis can be tricky to diagnose, because it shares symptoms with other medical conditions, including:
- ovarian cysts
- pelvic inflammatory disease
- irritable bowel syndrome
- irritable bladder
- certain musculoskeletal conditions
This may result in a misdiagnosis before you get an accurate endometriosis diagnosis.
Who’s more at risk of developing endo?
Some common risk factors may increase your chances of developing the condition:
- Family history of endo. Since endometriosis may have a hereditary link, you’re at a higher risk if a family member also has or had the condition.
- No previous childbirth. It’s more common to develop endo if you’ve never had a baby. Pregnancy may also temporarily decrease symptoms.
- Abnormal menstrual cycles. If you’ve got menstrual probs like periods that are heavier, longer, or shorter than average, you may be at a higher risk of developing endo. Starting your period before age 11 can also increase your risk.
Health conditions that have been linked to endo
- ovarian cancer
- breast cancer
- certain autoimmune disorders
- chronic fatigue syndrome
- asthma
- certain allergies
- sensitivity to certain chemicals, like phthalates
How bad can endo get? The stages of endometriosis
There are four stages — or types — of endometriosis. These are based on different factors like the size, amount, depth, and location of endometrial tissue.
Stage 1: Minimal
Minimal endo involves small lesions or wounds on your ovary, as well as shallow endometrial implants. In this stage, you may also experience inflammation in your pelvic area.
Stage 2: Mild
In mild endo, shallow endometrial implants and light lesions affect both your ovary and pelvic lining.
Stage 3: Moderate
Deep implants on your ovaries and pelvic lining develop in moderate endo, and more lesions may appear.
Stage 4: Severe
As the name implies, this is the most severe form of endo. In this stage, deep endometrial implants develop on your ovaries and pelvic lining. Lesions may also form on your bowels or fallopian tubes.
SOS: How to get a diagnosis
It’s important to see a doctor for an accurate diagnosis so you can get a treatment plan in place.
During your appointment, be prepared to share your detailed personal and family health history. Your doc may also do a general health assessment to check for any signs of endo.
To figure out whether you have endometriosis, your doc will likely do one or more of these tests:
- Pelvic exam. Your doc will do a manual exam inside your vaginal canal to feel for lurking endo indicators like cysts or scar tissue.
- Ultrasound. Using either a transvaginal or an abdominal ultrasound, your doc will get images of your reproductive organs to see if there are any physical signs of endo.
- MRI (magnetic resonance imaging). This gives your doc detailed images of your insides, but it isn’t always necessary. You’re more likely to get an MRI to prep for surgery to remove endo tissue.
- Laparoscopy. During this minor surgery, your doc will make a small incision to look for endo signs directly inside your abdomen. This procedure can also be used for removing endometrial tissue.
How to deal: Endometriosis treatment options
Endo has no cure, but it’s possible to treat and manage your symptoms. Your doctor will work with you to determine what’s best for your individual needs.
OTC pain meds
While they’re not effective in every case, over-the-counter meds like NSAIDs (nonsteroidal anti-inflammatory drugs) and acetaminophen (Tylenol) are a simple option for managing endo pain.
Just make sure you’re not overdoing the recommended dose. This can really mess with your stomach.
Hormone therapy
Hormone therapy can help manage pain and regulate hormonal changes that promote tissue growth. This treatment may also help stop the progression of endometriosis.
Hormone therapy options for endo include:
- birth control pills
- gonadotropin-releasing hormone (GnRH) meds
- progesterone and progestin therapy
- aromatase inhibitors
Danazol
Danazol is a hormone medication used to stop menstruation and ease endo symptoms.
Danazol doesn’t stop endometriosis from progressing, and it comes with some side effects, such as acne and hirsutism (abnormal hair growth). It can also cause fetal development issues, so you can’t take it if you’re pregnant or could become pregnant.
Conservative surgery
Conservative surgery is used to remove or destroy endometrial growths without damaging or removing your reproductive organs. The most common of these surgeries is a laparoscopy.
During a laparoscopy, a surgeon makes small incisions in your abdomen to remove growths. They may also burn or vaporize the growths using a laser.
Conservative surgery is recommended if you’re trying to get pregnant or if your symptoms aren’t responding to hormonal treatments.
Hysterectomy
Usually recommended only as a “last resort” treatment, a hysterectomy involves removing some or all of your reproductive organs. This includes your uterus and cervix, as well as your ovaries or any visible implant lesions.
A hysterectomy is irreversible, and you won’t be able to get pregnant after this surgery. If you really want to have kiddos one day, consider getting a second opinion before moving forward.
Can you have endometriosis complications?
Along with potentially painful symptoms, endo is also rife with possible complications.
Endometriosis complications can include:
- infertility
- depression
- anxiety
- ovarian cysts
- development of scar tissue or adhesions
- intestinal or bladder complications
- increased risk of ovarian cancer or endo-linked adenocarcinoma
Talk with your doctor if anything seems “off” with your endo or if you start experiencing severe pain, unexpected bleeding, or symptoms you haven’t had before.
Endo support is out there ❤️
Endometriosis doesn’t just take a physical toll. Fertility issues, frustration, fear, and chronic pain can also affect your mental health.
But remember, you’re not in this alone. Talking with a licensed therapist or joining support groups can help.
Check out these resources for help finding an endometriosis community:
tl;dr
If you have chronic period pain, don’t be afraid to talk about it with a doctor.
Endometriosis is a chronic condition in which endometrial tissue grows outside your uterus. It can cause pain, discomfort, and a variety of complications, including infertility.
Anyone with a uterus can develop endo, but certain factors, such as genetics and period problems, can put you at higher risk.
Once you get a diagnosis, it’s important to monitor your symptoms. We don’t know exactly what causes endometriosis, and there isn’t a cure, but it’s possible to manage the condition.
Your doctor may recommend medications, hormone therapy, or even surgery. Treatment is based on your unique needs. Resources are available to help you manage your endo pain and any complications.
0 Commentaires