Sometimes, you wake up and your hands go, “You know what? I’m not quite done yet — I’ll join you in a bit.” But why do you experience numbness in your hands while you’re sleeping?
Numb hands aren’t too bad compared with some other things you could wake up with (like a stranger you married in Vegas… or a horse’s head).
Waking up with pins and needles in one or both hands is really common. Most times it’s nothing to worry about — maybe you slept in the wrong position. (Seriously, how is Homo sapiens this high up the food chain?)
But a bit of seemingly innocent muscular white noise could also signal an underlying health condition that needs further attention.
In this article, we’ll look into reasons your hands can sleep through the alarm clock, what you can do about it, and when you should seek medical attention.
What causes pins and needles when you’re asleep?
Waking up with pins and needles in your hands (and other areas) happens for a number of reasons. Here are 11 of ’em:
- nerve compression
- diabetes
- carpal tunnel syndrome
- cervical spondylosis
- thoracic outlet syndrome (TOS)
- peripheral neuropathy
- abnormal sleeping position
- side effects of chemo and other medications
- vitamin B12 deficiency
- alcohol use disorder
- ganglion cyst
11 causes of numb hands and fingers when you’re asleep
There are dozens of reasons you might wake up with numb hands. These range from minor annoyances like bad sleep posture to serious health problems like diabetes and chemotherapy side effects.
1. Nerve compression
If your nerves get squashed, pinched, or squeezed (in other words, compressed), that’s nerve compression. No fancy Latin here.
You may know it by its alter ego. You ever had a trapped nerve? Congratulations, you know what nerve compression feels like!
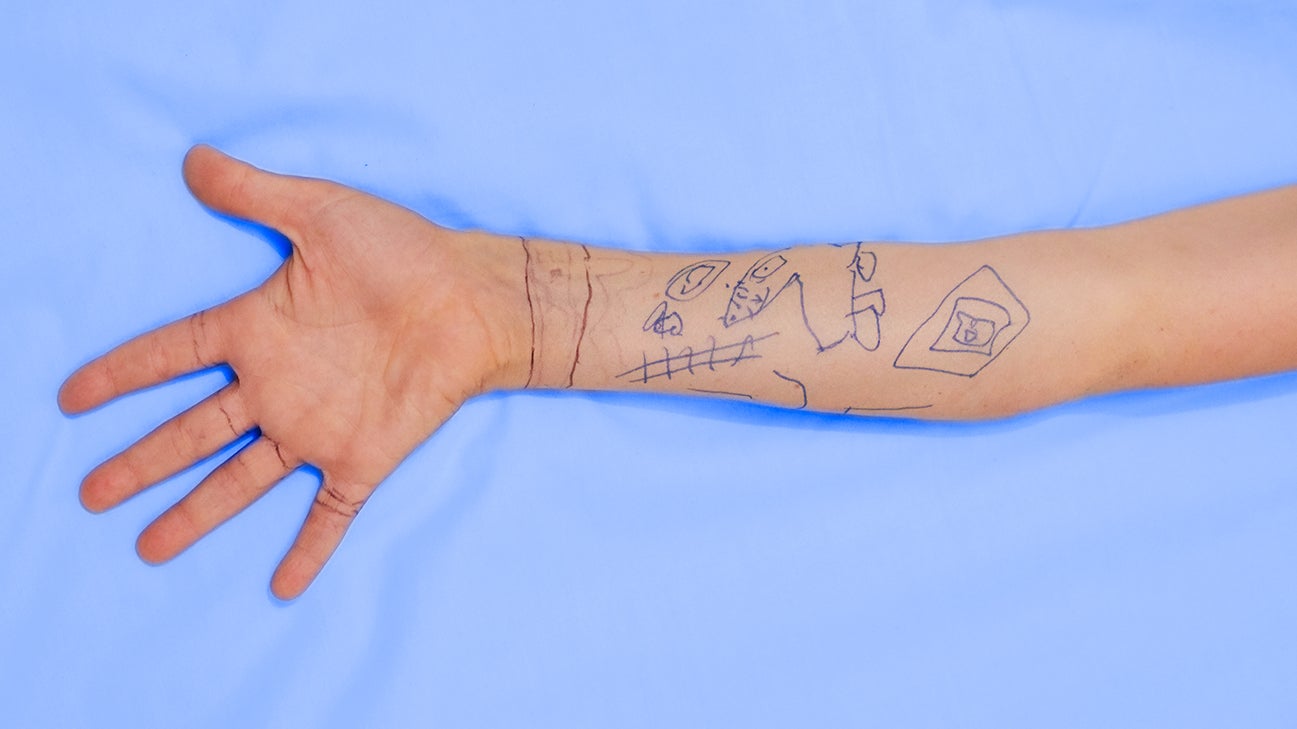
There are three main nerves in your arm and hand that cause numbness when compressed: the ulnar, median, and radial nerves.
Nerve compression is a symptom of other conditions or a result of an injury. We’ll cover the hand-relevant causes in more detail below. However, not all hand numbness is due to nerve compression.
2. Diabetes
More than 34 million peeps in the U.S. live with diabetes. It’s a manageable chronic condition but causes symptoms even when you’re getting treatment.
Diabetes complications can lead to swelling in areas that put pressure on critical nerves and veins. Some cases of carpal tunnel syndrome happen for this very reason.
Diabetes can also cause numbness as a result of nerve damage. Not only does diabetes squeeze your nerves, but it also basically makes your blood erode them, which is no picnic.
Nerve damage in the limbs, aka peripheral neuropathy, is a common symptom of both type 1 and type 2 diabetes. It’s so common that up to half of all people with diabetes experience it. Usually, it affects the feet and legs, but peripheral neuropathy can also occur in the arms and hands.
Diabetes increases your blood sugar, and prolonged exposure to high blood sugar (and fats such as triglycerides) erodes both your nerves and the tiny blood vessels that feed them.
Symptoms are usually worse at night, which explains why you notice the pins and needles when you wake up. Peripheral neuropathy is serious. The numbness can soon become a much more painful burning sensation, blisters, and sores. At its worst, it may lead to amputation of limbs.
Sound dramatic? You bet it does. Diabetes is a dramatic illness, responsible for more than 85,000 deaths in the United States every year. If you’re experiencing hand numbness with other diabetes symptoms, consult a medical pro immediately.
3. Carpal tunnel syndrome
Carpal tunnel syndrome (CTS) causes numbness in the hands because of compressed nerves. Specifically, the median nerve. Super specifically, somewhere near the wrist. You’ve probably heard of CTS.
Your carpal tunnel is a passageway of ligaments and bones that holds the median nerve and the tendons that bend your fingers. When the carpal tunnel swells up, it puts pressure on the median nerve, causing numbness and pain.
If the tingling you experience is focused in your thumb, index finger, middle finger, and the palm of your ring finger, it’s highly likely CTS is working its sneaky tricks.
CSI: RSI
CTS is commonly associated with repetitive strain injury (RSI). RSI is common in folks who work in offices or generally spend a lot of time smashing keys and clicking mice.
Construction workers and other people who make their living using vibrating machines should also be aware of the risks.
Always position your wrist safely and comfortably when typing or using heavy/shaky gear. Take regular breaks too — and stretch when you can. It’s called repetitive strain injury for a reason.
Injury (repetitive or otherwise) isn’t the only cause of CTS. Some other causes are:
- diabetes
- thyroid dysfunction
- fluid retention issues during pregnancy or menopause
- high blood pressure
- autoimmune disorders
4. Cervical spondylosis
Cervical spondylosis is both fun say over and over really fast and an age-related spinal condition.
In the United States, more than 85 percent of folks over 60 years of age have some kind of cervical spondylosis. The condition’s name is a general term for age-related breakdown of the cervical vertebrae (the neckbones).
Symptoms of cervical spondylosis include:
- stiff neck
- back/neck pains
- dizziness
- headaches
- numbness pretty much anywhere in your body
Numbness from cervical spondylosis happens when the disks between vertebrae erode and shift out of place. This exposes or compresses nerves in the spinal column.
But aging isn’t the only cause of cervical spondylosis. Spinal conditions that can lead to it include:
- Degeneration: a general wearing down of spinal disks in the neck
- Herniation: when one of the disks actually tears or cracks (yikes)
- Osteoarthritis: a condition that degenerates the cartilage between bones more quickly than normal aging does
- Bone spurs: when the bones exposed by reduced/moved cartilage scrape together and grow ridges
Cervical spondylosis can progress to cervical spondylotic myelopathy (CSM). This is serious damage to the vertebrae that protect the central nerves in the spinal column. CSM causes extra symptoms, including:
- numbness and/or tingling in the limbs
- difficulties with bladder and bowel control
- lack of sensation and control in the feet, which causes trouble walking
- damage to nerves responsible for fine motor skill coordination in the hands, making tasks like writing a real challenge
There’s no cure for cervical spondylosis, but physical therapy can make it easier. Your doc might also prescribe pain meds for some much-needed relief.
5. Thoracic outlet syndrome (TOS)
Your armpits are a hotbed of super important veins, nerves, and arteries that run from your neck to the area through the gap between your rib cage and collarbones.
The gap they run through is the thoracic outlet. You’ve probably already guessed that thoracic outlet syndrome (TOS) is when the situation in the thoracic outlet starts heading south.
TOS happens when the muscly bone gap compresses, squashing the nerves and blood tunnels within. There are three main flavors of TOS:
- Neurogenic TOS happens because of compression in the nerves connecting the neck and arm.
- Arterial TOS is due to a compressed artery.
- Venous TOS happens when a vein is compressed.
The tingling and numbness caused by TOS are accompanied by other symptoms, including:
- pain and discomfort
- swelling
- a bluish tint to the skin
- tiredness in one or both arms
In rare cases, TOS can also lead to a withering of the thumb pad.
A good way to test for TOS is to hold your arm upward. Symptoms get worse if an arm is elevated. So if the tingling/numbness gets worse when you’re trying to get your teacher’s attention because you totally know the answer, it may be TOS pulling the strings.
Physical therapy is the most common treatment for TOS. A doctor can also prescribe Botulinum toxin injections (Botox to its pals) if physical therapy doesn’t work.
If you have super severe TOS, you may need surgery.
6. Peripheral neuropathy
Neuropathy is the breakdown or damaging of nerves. Peripheral neuropathy is nerve damage in, well, your peripherals — your hands, feet, arms, and legs.
Nerve compression damages nerves by squeezing or constricting them. Neuropathy is any kind of damage that erodes, severs, or destroys the nerves.
Nerves are complex and delicate instruments that can become damaged or disrupted in many ways. Diabetes isn’t the only condition that can cause peripheral neuropathy.
Docs have identified well over 100 causes of peripheral neuropathy, commonly including:
- injury
- diabetes
- vascular problems
- systemic autoimmune diseases
- hormonal imbalances
- kidney and liver disorders
- nutritional or vitamin imbalances (especially a shortage of vitamin B12 or excess vitamin B6)
- alcohol use disorder
- medication side effects
- certain cancers and benign tumors
- certain chemotherapy medicines
- infections
Peripheral neuropathy is a complication or symptom of an underlying condition. Treatment depends on the nature of the cause.
7. Your sleeping position
It seems flippant to say you might have slept on it funny, but… you know… you might have slept on it funny.
Sleep posture is important. As health issues go, this isn’t one you should sleep on. A bad sleeping posture can put pressure on nerves and key blood vessels. This could be behind the nocturnal numbness in your fingers.
Nerve and vascular compression over a long period is a surefire way to cause numbness, tingling, and even pain or discomfort.
The return of the blood after a bout of restricted flow causes the spike in tingles as you wake up.
Try being conscious of your posture (especially of your arms, wrists, and hands) both as you fall asleep and as you wake up. It may be that you simply need to adjust your position to stop the pins and needles.
8. Side effects of chemo (and other medications)
Several medications list peripheral neuropathy as a side effect. Chemotherapy medications carry a risk of nerve damage.
Chemotherapy-induced peripheral neuropathy (CIPN) affects 30 to 40 percent of people who undergo chemotherapy.
If you’re not undergoing chemotherapy you’re not at risk of developing CIPN. If you are, here are the symptoms associated with it:
- pins and needles, complete numbness, or a tingling sensation
- sharp/stabbing, burning, or shock-like pain
- fine motor skill problems (when tasks like writing and texting become difficult)
- problems gripping or holding on to things
- clumsiness, as well as general balance and coordination problems
- weakness
- oversensitivity to touch
- temperature confusion (when your body doesn’t react appropriately to hot or cold temperatures or you have trouble telling which is which)
- reduced or slowed reflexes
- dysphagia (trouble swallowing)
- jaw pain
- hearing loss
- constipation
- trouble urinating
If you’re going through chemo and experiencing any of the above, contact your doctor immediately. CIPN is serious. In severe cases, it can lead to paralysis, organ failure, or death.
Chemo medications that can cause CIPN
Not all chemotherapy medicines carry a risk of CIPN. Cancer experts still don’t know exactly why these medicines causes it. These chemo drugs carry a far greater risk of CIPN than others:
- carboplatin
- cisplatin
- etoposide
- halaven (eribulin)
- ixempra (ixabepilone)
- jevtana (carbazitaxel)
- kyprolis (carfilzomib)
- oxaliplatin
- pomalyst (promalidomide)
- revlimid (lenalidomide)
- taxotere (docetaxel)
- thalomid (thalidomide)
- velban (vinblastine)
- velcade (bortezomib)
- vincristine
- vinorelbine
If your doc prescribes a course of these, ask them about how to reduce the risk of side effects. And follow your dosage recommendations to the letter.
Other medications
There are other, non-chemo drugs that can cause peripheral neuropathy (and the associated numb hands). If you’re concerned, check the label or informational booklet that came with your medication.
Here are some other types of medication that list neuropathy as a side effect:
- Anticonvulsants. Some common anticonvulsants are clonazepam (Klonopin), lamotrigine (Lamictal), divalproex (Depakote, Depakote ER, and Depakote Sprinkles), topiramate (Topamax), gabapentin (Neurontin), and levetiracetam (Keppra).
- Some heart meds and blood pressure-reducing meds. These include amiodarone (Pacerone, Cordarone) and hydralazine (Apresoline).
- Certain antibiotics. These include metronidazole (Flagyl) and fruoquinolones (Cipro, Levaquin).
9. Vitamin B12 deficiency
Your body uses glorious vitamin B12 to maintain function in your brain and central nervous system, as well as for DNA synthesis. Without B12, repairing damage to your nerves becomes a massive challenge. Like, an old-school-Nintendo-boss-level challenge.
This causes all kinds of issues with both the nervous system and the production of crucial blood cells.
If you experience any of these symptoms alongside your fuzzy morning fingers, it may be a sign of B12 shortage:
- pale or jaundiced skin
- weakness and fatigue
- balance or mobility problems
- a swollen, red tongue and/or mouth ulcers
- breathlessness
- dizziness
- blurry vision
- mood swings
- high temperature
Vitamin B12 (which is sometimes referred to as cobalamin) is a key ingredient in the production of myelin. Myelin is hella useful for insulating your nerves and generally maintaining the wiring of your brain.
If you have a B12 deficiency, your body can’t make enough myelin. Without protective insulation, your nerves are open to damage. This is why B12 deficiency can cause two seemingly unrelated symptoms like a swollen tongue and mood swings. It potentially compromises the entire nervous system.
Vitamin B12 deficiency has a number of possible causes. Age, genetics, and medical conditions like gastritis and autoimmune diseases can all be triggers.
Consult a medical professional if you’re showing symptoms. It could be treatable with dietary supplements but can get serious quickly if left unchecked.
10. Alcohol use disorder
Alcohol damages pretty much everything in your body. Your nervous system is definitely no exception. Excess alcohol intake can cause alcoholic neuropathy.
Alcoholic neuropathy causes pains and tingles for many people with alcohol use disorder. The mental health aspects of the condition often lead to poor self-care, resulting in dietary shortcomings.
Vitamin and mineral deficiencies make the sensations of alcoholic neuropathy much worse for lots of the folks trying to live with the condition.
If you believe your numbness may be due to your alcohol intake, speak with a doctor. If you’re worried that it may be part of a larger problem you have with alcohol consumption, there are plenty of support groups, licensed counselors, therapists, and medical detox facilities available.
Don’t suffer in silence
If you have alcohol use disorder, remember: You’re never alone, and it’s never too late to reach out.
Get in touch with the National Institute of Alcohol Abuse and Alcoholism helpline at 1-800-662-HELP (4357) if you need help breaking the cycle.
11. Ganglion cyst
For a condition whose name is literally a combination of the words “gang,” “lion,” and “cyst,” ganglion cysts are surprisingly harmless.
A ganglion cyst is a lump that can grow on your joints or tendons, including on your wrists. If it presses on a nerve, it can cause a bit of pain or numbness. It may also hurt a bit if you press on it.
However, there are two bits of awesome news about ganglion cysts that everybody should know:
- Like all the best lumps, they’re noncancerous.
- They usually resolve without treatment.
It’s always a good idea to consult a medical professional about any lumps you find. Just because it walks like a ganglion cyst, talks like a ganglion cyst, and lives on your wrists like a ganglion cyst doesn’t mean it is one.
If a ganglion cyst is behind your symptoms, there’s a good chance you won’t need treatment. Your pins and needles will recede when the cyst does. Dope.
Other health conditions
The above examples cover some of the most common reasons for numbness in the hands. But those aren’t the only possible causes. Dozens of conditions can cause numbness in your hands or fingers.
Some other possible causes of your waking wobble fingers include:
- rheumatoid arthritis
- hypothyroidism
- HIV
- syphilis
- multiple sclerosis
- Lyme disease
- Sjögren’s disease
- Guillain-Barré syndrome
- Raynaud’s phenomenon
- lupus
Numbness when sleeping (in more than just your hands and fingers)
You’re a smart cookie, so you’ve figured out by now that there are loads of reasons for nocturnal numbness.
A doctor can and should help you work out the cause. It’s best not to self-diagnose. But it could help your doc greatly if you can specify where in your body you get pins and needles, especially if it’s not just in your hands.
Waking up with numb hands and arms
Most of the conditions that cause numb hands can also cause numb arms. Your hands are attached to your arms, so it stands to reason that most things that impact your hands could extend into your arms.
What’s important is how much your arm tingles in comparison to your hand and how far up your arm the tingles reach.
Key culprits for hand and arm numbness are:
- cervical spondylosis
- peripheral neuropathy
- TOS
- alcohol use disorder
Waking up with numb hands and feet
If both your hands and your feet have pins and needles, some kind of neuropathy is probably at play.
Waking up with only one numb hand
If only one hand is numb, then your pins and needles are most likely related to nerve compression. Sleep posture, TOS, and carpal tunnel syndrome are likely causes.
Ganglion cysts are usually painless. But if a cyst presses on a nerve — even if the cyst is too small to form a noticeable lump — it can cause pain, tingling, numbness, or muscle weakness.
When to see a doctor about waking up with numb hands and fingers
You don’t have to worry about occasional post-snooze hand numbness if you:
- have no underlying conditions
- are not undergoing chemotherapy
- don’t take any regular medication
You need to see the doc only if adjusting your sleeping position hasn’t relieved the numbness or if the pins and needles stick around and get worse.
If you do experience numb hands when waking up and you have a preexisting condition like diabetes or are undergoing chemotherapy, consult your doctor immediately.
Age can also be a factor — folks in their golden years should pay closer attention to numb hands than their young whippersnapper counterparts need to.
Call 911 (or your local emergency number) immediately if you experience a sharp or sudden numbness followed by:
- stabbing pains
- slurred speech
- weakness or paralysis
- a headache
These symptoms could indicate a stroke.
Treatments for hand numbness
How you treat your prickly palms and pointers depends entirely on why they’re prickling.
For example, adjusting your sleep posture is fine and dandy for nerve compression, but it won’t do much to take the edge off diabetes-related peripheral neuropathy. And it doesn’t account for midsnooze shifting.
If your hand numbness ends up requiring treatment, it will probably be as part of a treatment program for the underlying condition. Your doc may recommend any of these methods to make your pins and needles less pins-and-needlesy:
- Exercise. This is particularly good for treating carpal tunnel syndrome.
- Over-the-counter pain medications. Nonsteroidal anti-inflammatory drugs like ibuprofen or aspirin can be prescribed to reduce inflammation that may be compressing nerves.
- Splints/wrist guards. If you’ve damaged nerves in your arm, a splint or wrist guard can take the pressure off of them and allow them to heal.
- Topical treatments. Lidocaine patches or capsaicin cream can work. They relieve a lot of the pain associated with peripheral neuropathy.
- Vitamin B12 supplements. Even if you’re not directly supplementing a B12 deficiency, strengthening your body’s ability to repair and insulate nerves goes a long way toward relieving discomfort from neuropathy.
- Antidepressants and antiseizure meds. Some antidepressants and antiseizure drugs can also relieve nerve pain.
- Surgery. Surgery is always an option if nonsurgical treatments aren’t effective. The exact procedure depends on the cause.
Managing numbness yourself
You should always consult a medical professional if your numbness happens regularly, interferes with daily life, or might have links to a larger condition like diabetes.
If it’s more of a mild nuisance than a medical concern, there are a few ways you can manage and relieve symptoms:
- Take regular breaks from activities like typing or writing (anything that’s repetitive or strenuous for your wrists, hands, or forearms).
- Do plenty of exercises to strengthen the muscles in your arms, hands, wrists, and fingers.
- Eat a balanced, B12-rich diet (and take vitamin B12 supplements if necessary).
- Be mindful of your sleeping posture. Adjust your sleeping position if the numbness persists.
Takeaway
Numb hands when you wake up are normally nothing to worry about. But that doesn’t mean you should ignore them, since they could be a sign of a more serious underlying condition.
If you have a clean bill of health (no diabetes, chemo, etc.), be mindful of numbness in your hands when you wake up, but don’t stress about it.
Consult your doc if self-management techniques make no difference, the numbness gets worse or becomes painful, or you start experiencing other symptoms.

0 Commentaires